The hospital waiting list in England just hit a new high of 7.2 million people. And for the first time in 106 years, the Royal College of Nursing has decided to strike after more than 300,000 members voted for industrial action, demanding better pay and citing concerns for patient safety. The strikes are set to take place from the 15th to the 20th of December. Rising East spoke to an NHS A&E Paediatrics nurse and an A&E patient to bring you first-hand accounts of the developing crisis.
Since the pandemic it has been difficult to book GP and doctor’s appointments. Many patients’ conditions worsen whilst waiting for an appointment, so they end up going to A&E out of desperation. This surge of last resort patients on top of the expected A&E emergencies and staff shortages has seen A&E wait times skyrocket. In emergency departments, just 68.9% of patients in England were seen within four hours last month, down from 69.3% in October and the worst performance on record.
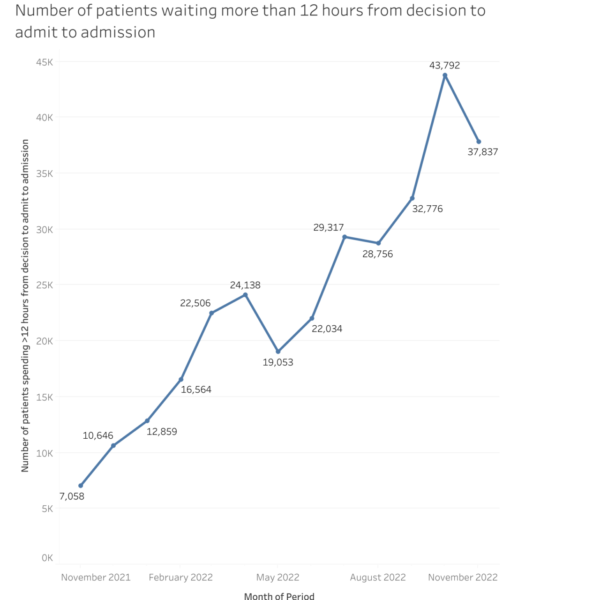
The waiting doesn’t stop once patients are told they are being admitted for further assessment and/or treatment. NHS England’s A&E Attendances and Emergency Admission statistics reveal that the number of patients waiting more than 12 hours from the decision to admit them to being admitted has increased by 30,779 (436%) from November 2021 to November 2022.
The nurse
We spoke to NHS A&E paediatrics nurse, Natasha (name changed for anonymity reasons), about the reality of working in A&E under the current NHS crisis. Referring to the pressure and conditions in her ward, Natasha said, ‘It’s the worst it’s ever been’. She has seen wait times for a bed or to be seen by a doctor reach 15 hours in paediatrics and over 23 hours in adult A&E.
Natasha says that the number of paediatric patients is always higher in the winter because infants get coughs and colds that their lungs are not strong enough to handle. This means they ‘often end up on oxygen machines which makes them a HDU patient [a patient on a High Dependency Unit] and with the little number of staff and staff sicknesses, it’s hard to manage’. Natasha explained that the ratio of nurses to HDU patients is meant to be 1:2, but because of the pressure it is now 1:3 and sometimes 1:4. She said, ‘Because we have so many sick kids on the ward, there are 50+ more waiting in A&E which is just as unsafe’.
There is a justified focus on the impact all of this has on patients, but the impact it has on the people working on the ward is often overlooked. When asked about the impact on staff, Natasha said, ‘I can sense the ward morale being a lot worse. The ward is miserable and nurses are just exhausted’.
Last year, 25,000 nursing staff around the country left the Nursing and Midwifery Council, along with 47,000 unfilled nurse posts in the NHS. The nurses that stayed have decided to hold strikes this month. Natasha voted to strike, but her hospitals trust didn’t get enough votes to strike from its nurses. This means Natasha and her colleagues cannot strike; however, they can support other trusts at the picket line and will still benefit from any changes that come as a result. Natasha said they are striking for ‘better working conditions, better pay and just a better work life balance’. She continued, ‘No job is worth this amount of stress. Of course, it’s healthcare so it’s going to be scary and emotionally challenging, but it’s become too much now, and it just seems like the government don’t care.’.
The patient
We also spoke to A&E patient, Sophie, about her experience. After being advised by a 111 operator, Sophie went to an A&E unit at 10pm on the 6th of December with an excruciating twisting pain in her stomach. There was a queue out of the door just to get a ticket that allows people to go into the urgent treatment centre. In there they are assessed and given a coloured card (the colour of the card represents the urgency of the case) to take to A&E where they will have wait again to see a doctor. Sophie said, ‘We waited over an hour and did not move forward into the queue and did not even give anyone my name’. There were no seats and after telling a nurse that she could not stand any longer due to the pain, the nurse informed her that there were around 200 people waiting in the urgent treatment centre alone. Sophie had no other option but to go home and wait for a 111 clinician to call her back. It wasn’t until 8am the following morning that Sophie finally got a call back, despite being listed as urgent. She then headed back to the hospital where she was finally seen. Sophie said, ‘In total, I have waited around 15 hours to see a doctor from first attending hospital and reaching out to 111’.
After multiple tests it was discovered that Sophie was suffering from appendicitis and needed urgent surgery to remove her appendix before it ruptured. Adding to her stress even more, Sophie was shouted at by a member of staff when she asked if he could wait until her father was out of the room before he asked questions about her vagina and sex history. She requested another member of staff to sit in on the scan as she ‘didn’t feel comfortable with him being in the room’. After her scan, the head consultant apologised for the conduct of the staff member and reassured her that he had been spoken to regarding his behaviour. Despite this bad experience and all the waiting around, Sophie said that ‘the nurses here were so pleasant and made me feel really at ease’.
Regarding the NHS crisis, Sophie said, ‘I feel due to the intense pressure on the NHS from underfunding, overwhelming demand and understaffing, it is bursting at the seams. Nurses have been repeatedly apologising due to the long wait times which really highlights the system is broken. It is not the nurses’ fault, yet they feel responsible for the experience of the public. This is leading to nurses overworking themselves and burning out. It’s really sad to see.’.
When we first spoke to Sophie, she had been admitted for around 12 hours, waiting for a bed to free up at another hospital so that she could be transferred for surgery. Rising East caught up with Sophie again after her surgery for an update. The surgery was successful, and she is now recovering at home surrounded by friends and family.
To download free campaigning materials and learn more about how can support the Nurses on strike, head to: https://shop.rcn.org.uk/collections/free-campaigning-materials

